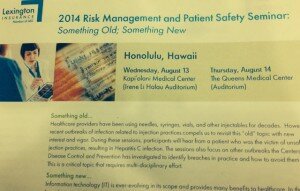
A Survivor reacts to a new outbreak

Recently West Virginia health authorities announced that a cardiac clinic is at the center of an investigation of a potential outbreak of viral hepatitis through unsafe injection practices. Johnny Robertson of North Carolina is a survivor of a similar outbreak and is an active advocate of injection safety. We are grateful to Johnny for his leadership in patient advocacy. Following is his reaction to the outbreak.
In January 2008, I heard the words, “You have hepatitis C.” This diagnosis changed my life completely.
I contracted hepatitis C during a stress test at a cardiology clinic in North Carolina in 2007. Later, it was revealed that a medical technician administered saline solution to a patient who was infected with this life threatening disease, then reused the same syringe to re-enter the vial. This contaminated the vial of medication with the virus. Subsequent patients who received an injection from the saline solution vial were exposed to the virus. Five patients were infected with the virus, but many more were exposed and were urged by the state health department to be tested.
Several weeks ago, West Virginia’s Department of Health and Human Resources sent letters to 2,300 people potentially exposed to hepatitis B, hepatitis C and HIV through cardiac stress tests at Raleigh Heart Clinic in Beckley. From the recent article (“Hepatitis cases linked to Beckley clinic likely caused by human error,” March 29), we know that 12 patients have been infected with hepatitis C or hepatitis B.
This tragic news strikes an eerily similar tone.
In addition to the dozen patients who have been infected, my heart breaks for the patients who sit and wait and worry while results from blood tests come back. I offer them my deepest support.
Outbreaks like this one oftentimes affect entire communities. Families and friends and colleagues are affected. They take a toll on the human psyche, and they are complicated and costly.
The truth of the matter is this could have been prevented. It did not need to happen.
Generally, healthcare in the United States is very safe. But sometimes, unsafe practices are used—brought about by ignorance, desire to cut costs, or the demand to see more patients in a shorter amount of time.
But there are efforts to educate both healthcare providers and consumers about the absolute need for safe injections in all settings.
I work alongside colleagues at Hepatitis Outbreaks’ National Organization for Reform and North Carolina’s One & Only Campaign. I am proud to serve as a spokesman for this award-winning campaign. I tell my story to healthcare providers throughout the state to help reeducate and advocate for injection safety, urging them to use “One needle, one syringe, and only one time!”
Patients need to have a voice in healthcare. No one in the United States should be infected with hepatitis C while receiving healthcare. My hope is to support those who are going through this very difficult time and allow the conversation to begin about tighter safety protocols, in West Virginia and elsewhere. There is help out there for those who need it. I know because I was once in this same situation.
Johnny Robertson